- [Joann] Hello, and welcome to our Webcast today
on the New AHRQ Surveys on Patient Safety Culture
Health Information Technology Patient Safety
Supplemental Items for Hospitals.
My name is Joann Sorra and I'll be the moderator
for today's Webcast.
I'm the Associate Director at Westat,
and I'm the Project Director for the contract
that supports the AHRQ Surveys on Patient Safety Culture.
Before we begin I have just a few
housekeeping details to go over.
If you're having difficulty hearing the audio
from your computer speakers you can switch the audio
selection by having WebEx call you at a phone number
you provide and you can then connect through your phone.
In the event that your computer freezes
at any point during the presentation
you can try logging out and logging back into the Webcast
to refresh the page.
Remember though, that you may just be experiencing
a lag in the advancement of the slides
due to your internet connection speed.
During this Webcast at any time you can use
the Q&A icon to ask questions or request help.
Again, at any time during today's presentation
if you're having technical difficulties
or have a question for our speakers
you can use this Question and Answer feature, Q&A.
Depending on the browser you're using,
your WebEx screen may look slightly different
than this slide.
So look for the Q&A icon and be sure
that the drop down option displays all panelists
for you to ask the question so our team can see it.
Feel free to share your name or organization,
or role when you type your question.
Today's session is being recorded and a replay
of today's Webcast and the slides will be made
available on the AHRQ Web site.
So now that we have some housekeeping items out of the way,
I'm very pleased to introduce our speakers
for today's Webcast.
We're pleased to welcome Rear Admiral Jeff Brady,
Physician and Director of the Center for Quality
Improvement and Patient Safety at the Agency
for Healthcare Research and Quality.
Dr. Brady also serves as a Assistant Surgeon General
in the Commission Corps of the U.S. Public Health Service.
He has served as the director of AHRQ's Center
for Quality Improvement and Patient Safety since 2014,
and led the AHRQ Patient Safety Research Program
from 2009 to 2014.
He leads a part of the agency that conducts AHRQ programs,
which include patient safety research
and the Surveys on Patient Safety Culture,
healthcare-associated infections prevention,
the patient safety organization program,
the National Healthcare Qualities and Disparities Report,
and the Consumer Assessment of Health Care Providers
and Systems, or CAHPS Program.
We're also pleased to have Dr. Tejal Gandhi,
who is the Chief Clinical and Safety Officer
for the Institute for Healthcare Improvement,
where she leads programs focusing on
improving patient and workforce safety.
Dr. Gandhi was President and CEO
of the National Patient Safety Foundation
from 2013 until 2017 when they merged with IHI.
She continues to serve as President
of the Lucian Leape Institute and holds an appointment
as an Associate Professor of Medicine
at Harvard Medical School.
Dr. Gandhi is a prominent advocate for patient safety
at the regional, national, and international levels
driving educational and professional certification efforts
and helping to create and spread
innovative new safety ideas.
She received her MD and MPH from Harvard Medical School
and the Harvard School of Public Health,
and trained at Duke University Medical Center.
And we also have Dr. Naomi Dyer Yount,
who is the Senior Study Director at Westat,
and an industrial organizational psychologist
with more than 15 years of experience
in organizational research and analysis.
Dr. Yount has been involved in developing
the database reports for AHRQ's Surveys
on Patient Safety Culture and has worked extensively
in analyzing and exploring data from the Hospital,
Nursing Home, Medical Office, and Community Pharmacy
Surveys on Patient Safety Culture.
She also conducted psychometric analyses for these surveys.
Dr. Yount is working on updating the Survey on
Patient Safety Culture for Hospitals, to create Version 2.0,
and recently worked on the development and release
of the Health Information Technology Patient Safety
Supplemental Item Set.
Many thanks to our speakers today, and without further ado,
Dr. Jeff Brady will be our first speaker.
Handing it over to you, Jeff.
- [Jeff] Great, thank you, Joann.
Just a quick soundcheck, can folks hear me okay?
- [Joann] Yes, we can, yes.
- [Jeff] Great, thank you, Joann.
I am really pleased to be introducing this topic
and also telling you just a bit about how
this patient safety culture and the surveys in particular
fit into our broader research programs here at AHRQ.
Just a brief background on our current priorities
on patient safety.
I think it's probably clear to many in the audience
that we focus on areas of greatest impact
so that while we have lots of research looking at
assessment of harm, epidemiologic perspective of
patient safety where most harm occurs,
we also transition through to solutions
and understanding broader foundational issues
like patient safety culture
that you'll hear more about today.
We are also very focused on extending patient safety
improvement to all health care settings.
Obviously a lot has happened in the hospital.
We're focused on a tool that is itself focused on
the hospital culture and HIT in particular.
However, our interests are quite broad
across the full spectrum of care and all settings.
HAIs are a particularly important topic for us,
as are all patient safety events and event types.
But in particular HAIs, we have more substantial funding
for that set of patient safety issues,
and with a particular focus on antibiotic resistance
and stewardship and related topics.
A lot of our work really takes into consideration
the capacity that we're trying to make use of,
and in fact help build within health care
to accelerate patient safety improvement.
A key example of that is communication and engagement,
not only between clinicians, but with patients,
recognizing those foundational factors
and the role they play in patient safety improvement.
And then within that same vein,
whatever our research is showing we want to
always translate that into feasible and useful solutions
and the simple way we describe that obviously
is making the safe thing the easy thing to do.
You've heard a little bit about the programs
that are in our particular center at AHRQ.
The first three are patient safety focused.
But the others actually are inclusive
of patient safety topics and in particular
the work that you're hearing today benefits
from some of the methodologic expertise we have,
not only within the agency, but in our extended
set of partners, the contractors, and grantees that we have.
So survey methodology and the importance
of making sure that we have the right level of rigor
and these tools in resources,
we get some efficiencies across our CAHPS Program,
which is itself a survey-based tool.
So just a little bit about how we try to make use
of, again, a broad range of expertise.
Turning now to the topic of patient safety culture
in particular, I think we all appreciate that
patient safety culture can be defined
as the beliefs, values, and norms that support
and promote patient safety within an organization.
These beliefs, values, and norms are shared
by health care providers and staff in that organization.
And the real key point and I think one of the main reasons
we're so interested in patient safety culture
is because it is one of the main factors that determines
behaviors that are rewarded, supported, expected,
and accepted within an organization.
So when an organization uses a resource like the SOPS survey
to measure patient safety culture they're in fact
measuring directly these behaviors, again,
that are rewarded, supported, and accepted.
It's also important to note that culture exists
at multiple levels from the unit level in a hospital
to the department at larger levels
all the way up to the hospital itself,
and then finally the system.
So these factors are all taken into account
based on the structure and the way that
the survey instrument is organized.
Just a little bit about the history of the program,
which began in 2001 with the development of
the Hospital Survey on Patient Safety Culture.
We released that survey in 2004.
That gives you a sense of the amount of energy, time,
and attention that was put in to making sure that
the survey performed as we wanted it to,
and that it in fact is something that folks
in operational settings can actually rely on
to guide their work.
We now have more four more SOPS surveys
that are available for the nursing home setting,
medical offices, also community pharmacies,
and finally the most recent in 2015
ambulatory surgery centers.
The patient safety culture concepts that are measured
across the surveys are similar.
But for each development of each of these different settings
the survey for each of these different settings,
the team has adapted and tailored the surveys themselves
to the issues that are specific to each setting.
That's been our really important part of the development,
because again, even though foundations are the same,
the actual delivery of care differs in ways
that actually are important for measuring safety culture.
We also support the SOPS databases,
the intake data from facilities that voluntarily
submit their SOPS survey data to AHRQ.
The database reports show aggregate results
and participating facilities can also receive
feedback reports that compare their own individual results
to those in the database.
The number of sites and provider and staff respondents
that are included in each of these databases
are shown here on this slide in the screen.
So over time this just becomes an increasingly rich resource
that appreciates in value with more participation.
So we're really excited about what this adds to the field,
and again, the value that it brings to interpreting
results at an individual organization level.
AHRQ has also recently released several supplemental item
sets that can be added to the end of existing SOPS surveys.
So there's the ability to tailor
the core survey with the supplements.
The Value and Efficiency supplemental item set
helps hospitals and medical offices assess
the extent to which their organizations
place a priority on and adopt practices to promote
efficiency, waste reduction, patient-centeredness,
and high quality care.
Another supplemental item set the SOPS,
the Health IT Patient Safety Culture supplemental item set,
the topic of today's Webcast, assesses how organizational
culture influences HIT and patient safety.
Obviously, HIT has enabled the health care system
in many different respects to become much more safer.
But we also are aware that there's increasing reliance
on information technology.
So I think this has grown, this resource has grown
out of recognition that it's important for hospitals
to understand the effects of HIT use on patient safety
including some of the unintended consequences of HIT.
So with that I'll turn it back over to Joann.
- [Joann] Thank you, Jeff.
That was a great introduction to the SOPS surveys.
Now we're gonna transition to Dr. Tejal Gandhi,
who's gonna talk about optimizing the use
of health IT to improve safety.
Dr. Gandhi.
- [Dr. Gandhi] Thanks, Joann.
I'm gonna talk about, as Jeff really alluded to
in his comments, the importance of the use
of HIT to improve patient safety,
and how we really need to work to optimize it,
and hopefully then make the link to the reason
why this cultural assessment is is important.
At the National Patient Safety Foundation
a couple of years ago we had done a report
called Free From Harm.
It was really intended to look at where we've been
in patient safety and where do we need to go.
One of the key components to this report
was really eight recommendations that we
came together with an expert panel to create
around how do we accelerate our progress
in patient safety.
Those eight recommendations are listed here.
The first, and actually these are not in any
particular order, except for the group very unanimously
felt that the first should be the first,
was around ensuring that leaders establish
and sustain a safety culture.
Jeff spoke about the importance of that.
But the ace was ensure that technology is safe
and optimized to improve patient safety.
One of the reasons that this ended up as a recommendation,
we were really trying to develop foundational
recommendations to improve foundational areas in safety,
and the fact that technology's is so ubiquitous now
in the health care that we deliver,
we felt like technology needed to be included
as a foundational concept that needed to be optimized,
again, to achieve quality and safety.
Here are some examples of why technology
has really been really critical
in trying to reduce errors.
Most people, when they see this, see Coumadin 4 milligrams,
and it's actually Avandia.
Here's another example of technology benefits
as well as challenges.
The complex ICU patients that need so many different
medications and drips and so forth,
and the technology with the pumps can really help
to make sure that we're delivering all those,
but also it's incredibly complicated to manage
and have opportunities for unintended errors as well.
This is, as we think about safety not just in hospitals,
but in the out-patient setting,
this is the complexity potentially of what patients
are having to deal with in the home.
And again, I think there are ways that technology
can potentially help to improve the medication management
process in the entire continuum of care.
There's been a lot written about how IT
can improve patient safety and in this article
the authors really talk about three major ways
that IT can improve safety.
First, by preventing errors and adverse events.
Secondly, facilitating a more rapid response
after an event has occurred.
And third, tracking and providing feedback
about adverse events.
There's many ways we think about that prevention
of errors piece, which was in the first bullet
in adverse events using IT.
There's many ways that technology
can really facilitate that prevention.
So technology can improve communication,
make knowledge more accessible,
require certain key pieces of information,
for example, requiring that a creatinine level
is present if you're ordering a drug that's cleared
by the kidney, assisting with calculations,
performing checks in real-time, assisting with monitoring,
and providing decision support.
So many ways that technology can help
with that error prevention.
We know from studies that have been published
that some technologies have the potential
to reduce errors significantly based on
some of those strategies I just went through.
These are some of the common examples that we talk about,
particularly computerized physician order entry,
or provider order entry, which has been around for a long
time and probably is the most well studied,
and has been shown to significantly
reduce medication errors, as well as things like
barcode technology, electronic prescribing systems,
handoff tools, and test result systems,
and referral systems.
These are the kinds of technologies that have the potential
to really reduce errors significantly.
We also know that technology has been adopted
at a rapid pace over the last several years.
These are older slides and this curve
has continued to move up.
But once incentives started, particularly
the adoption of EHRs in the ambulatory care setting
and EHRs in hospitals, really went up significantly.
With that significant rate of adoption
we've also started to see that there is a need
to optimize these systems.
As I mentioned, these systems have the potential
to reduce errors, like commute the computerized
physician order entry and so forth.
But unless they're implemented, actually designed
and implemented well, they may not actually
achieve all of those benefits.
So really, I think the attention over the last decade
was convincing people to adopt and implement
and I think our focus going forward is really
around how do we design and implement well
so we actually achieve the quality and safety benefits
that we think we should be achieving with these systems.
In order to do that we have to optimize these systems,
thinking about things like over-alerting, for example.
We all know that there's far too many alerts
in these systems.
So how do we reduce over-alerting in a smart way?
How do minimize variability across vendors?
Improve interoperability?
And also improve implementation?
A recent statistic from Leapfrog shows that 42% of hospitals
are failing to scan both the patient and the medication
for at least 95% of administrations.
The technology is there but if the patient and medication
aren't being scanned we're not gonna achieve
the benefits that we're hoping for.
And we know there can be unintended consequences.
One of the most commonly described one is copy and paste
or cut and paste and that fact that clinical documentation
have become very difficult to wade through
because of the prolific use of copy and paste.
Other unintended consequences are the fact
that we have medication lists and problem lists now
very visible in the EHR, but maintenance of those
has become a real challenge and we don't really have
robust processes to make sure that those lists
stay accurate in the system and are updated as needed.
There's been quite a bit of study about
unintended consequences and particularly around CPOE,
computerized physician order entry.
This is that study that really talked about the fact
that anytime you implement a new technology
you have to look for those unintended consequences.
CPOE, in particular, led to the ones you see here
in terms of changes in workflow that were not intended,
overdependence on technology, new errors that came in, etc.
So it's just a really important lesson to realize
that every new technology, although it may have great
benefits, also can potentially introduce new problems
that need to be identified and addressed.
This, I think, is one of the unintended consequences
that perhaps we didn't really foresee.
But we're seeing now that EHRs are being identified
as a source of burnout for our clinicians.
We hear about this both for physicians and for nurses.
So again, a really important unintended consequence
that needs to be addressed by thinking about design,
implementation, usability, etc.
This is a model that was published in 2010
called Sociotechnical Model.
It's really getting into the components
of how do you successfully implement.
As I said, we've focused on adoption,
but now we need to focus on
better implementation and design.
So this model talks about eight components
for successful implementation,
and you see the eight listed there.
It ranges from hardware and software,
which I think we focus on a lot on the software side,
but there's many other components as well
that are really critical.
I highlighted in red things related to people,
related to workflow, communication, and culture
as really being critical components
for successful implementation.
As I said, we often focus on the technology side,
but it's important to understand the culture,
people, communication pieces, etc. are also
really critical for successful implementation.
This is why I think the HIT culture
is critical to HIT success.
We need to create a culture of HIT safety
that's a critical foundation
to improving safety using technology.
So what do I mean by that?
Things like is our organization open to hearing
about HIT-related safety issues?
Some of those unintended consequences?
Is there feedback about safety issues?
If I report a problem with the system
do I hear back about what's been changed or not changed?
Is there punishment and blame?
There's many strategies that exist to make culture change
that can be relative to HIT.
For example, having robust reporting systems
that are able to capture HIT-related issues,
doing walkrounds to identify technology-related problems,
particularly in times of significant implementation.
This need to create a culture is really critical
for HIT implementation and it's great
that Westat and AHRQ have worked to develop a tool
to actually help measure where your HIT culture is,
which will be, I think, a significant advancement,
especially for organizations that are both
in the middle of adopting, about to adopt,
and have even gotten past adoption of some
of these major systems to understand how
their staff really feel about the way technology
is managed in the organization.
With that, I will pass it back to you, Joann.
- [Joann] Great, thank you so much, Tejal.
We've had a great background about the AHRQ Surveys
on Patient Safety Culture and about use of Health IT
as it relates to culture and now we're gonna hear
from Dr. Naomi Yount, who's going to introduce
the AHRQ Survey on Patient Safety Culture
Health IT Patient Safety Supplemental Item Set.
Naomi.
- [Naomi] Thank you, Joann.
I'm gonna talk with you about the development
of the Health IT Patient Safety Supplemental Items,
and share results from a recent pilot study we conducted.
Westat under contract with AHRQ did design
a supplemental item set that can be added
to the end of the Hospital Survey on Patient Safety Culture.
The goal of the item set was really twofold
to raise awareness about the impact of Heath IT
on patient safety, and assess how culture influences
Health IT and patient safety.
Our development process for that item set
followed our standardized process
for the SOPS surveys in general.
The first thing we did was review literature
and existing surveys to see what's out there
and what the key issues were.
We also identified technical experts
and formed a technical expert panel.
We interviewed experts in the field,
as well as providers and staff to get
the different perspectives of Health IT and patient safety.
From these steps we identified key thematic areas
that are important for culture
and Health IT in patient safety.
From those areas we developed draft items,
and we cognitively tested those items.
So that means we went out to people who would likely
take the survey, providers and staff,
and made sure they were understanding the items
the way that were intended.
We made edits to those items based on those tests,
and it was an iterative process where we went back
then out and cognitively tested more
until we had a set of items
that we were pretty confident about.
Then we went and got more input along the way.
We were getting input from our technical expert panel.
We agreed on a set of draft items.
We pilot tested them.
We conducted psychometric analyses
to look at the reliability of the items,
the variability.
And then we shared those results with our technical
expert panel and finalized the items,
which were released this year in March.
We had about five topic areas.
We had patient safety and quality issues which
really get at some of those unintended consequences
Tejal was just talking about.
We had two composites, an EHR system training
of three items,
EHR system support and communication, three items,
and then the rest are single item measures
revolving around workflow and work process,
and an overall rating on your EHR system.
In sum there were 16 items.
The one item that's not listed here
is a filter item that's at the beginning
that asks do you use your hospital EHR system
to enter or review patient information?
Because the Surveys on Patient Safety Culture
are often administered to all staff,
this filter question was added so that staff
who are not using the EHR could skip out of the questions.
We did the pilot test in 44 hospitals in the Spring of 2017.
We had a 42% response rate, about 15,000 respondents.
Of those 15,000 respondents 69% said yes
to the filter question that they use their hospital's EHR
to enter or review patient information.
The first set of items was really about
the patient safety and quality issues.
They were asked in the past three months
how many times did you discover these types of issues,
the first one being incomplete
information in the EHR system.
We see that 66% of respondents found or discovered
incomplete information in the EHR system
at least one time in the past three months.
Also in the survey at the very end of the survey
was an open-ended comments box.
So after they took the Hospital SOPS
and the supplemental items they could do any open-ended
comments they wanted to talk about other issues
in their hospital and I'll just provide some sample
comments as we go through some of these different issues.
Some sample comments for incomplete information,
we see here "I would have to say I find incomplete charts
almost all the time."
"There is still often missing information
that affects patient care."
The next item we see 64% of respondents indicated
that information was hard to find.
Some sample quotes here are "There are way too many places
to chart things and it's very hard to find information."
"We are using three different computer systems
for each patient."
"The information is very fragmented and hard to find
and put all in one place."
61% of respondents discovered information was not accurate.
Some sample quotes are "A lot of the medication lists
are either wrong or patients are having to call us back
to update their medication list."
"I do a lot of chart reviews and I frequently find
wrong information in physician progress notes."
29% of respondents discovered incorrect information
was copied and pasted.
Some sample quotes here are "Physicians sometimes
copy and paste incorrect information in notes."
"I think the errors in the charting occur
when people get in a hurry and copy and paste."
Finally, we see 32% of respondents said that information
was entered into the wrong patient health record,
or they discovered that it was entered into
the wrong patient health record at least one time
in the past three months.
Just one simple quote here is "Patient information
is scanned in the wrong patient chart.
I notify the appropriate person of these errors."
One of the composites was EHR system training.
We see that the composite score,
which is basically the average
of the items scores is 64% positive.
By percent positive, it means that they strongly agreed
or agreed with the item.
This composite is comprised of three items.
We are given enough training on how to use our EHR system.
Training on our EHR system is customized to our work area
with the highest percent positive at 67%.
We are adequately trained on what to do
when our EHR system is down at 62% positive,
or 62% strongly agreeing or agreeing with that item.
Some sample comments are "There is not formal training
for the EHR, you learn as you go."
"I have not been trained at all on how to use this program.
It seems no one has the time of day
to give me any training."
"No one really knows what the requirements are
for using downtime forms."
The other composite is on
EHR system support and communication.
It has a 50% positive.
It's got 50% positive,
which is a little bit lower than the other one.
We see problems with our EHR system
are resolved in a timely manner.
55% of people answered strongly agree or agree.
39% answered positively to: We are asked for input
on ways to improve our EHR system.
And 55% answered positively to: We are made aware
of issues with our EHR system that could lead to errors.
Some sample comments here are "We would like more
responsiveness by IT in making adjustments
to our electronic charting format."
"I wish that nurses would be consulted more frequently
on how to improve the EHR."
"Changes are made to our charting, and nothing is said.
We find out because we open the chart
and find new fields, new pages, new requirements."
Then we have a set of three single item measures
that revolve around workflow and work process.
The first one is: There are enough EHR workstations
available when we need them. Where 69% strongly agreed
or agreed with that item.
Now we have two negatively worded items
or reverse coded items, which means that to be a positive
response they have to disagree with the question.
The first one is: Our EHR system requires that we enter
the same information in too many places.
Where we see only 21% strongly disagreed
or disagreed with that item.
The next one--There are too many alerts or flags
in our EHR system. Where again, only 37% strongly
disagreed or disagreed with that question.
Some sample comments for this one are
"We need more portable workstations
or a computer in every room."
"Our EHR has too many places that we have to double
document information such as vitals, pain intake
and output, that could lead to mistakes."
"Everyone just leans to accept they will need to override
so many alerts and warnings that people tend not
to read them and miss significant drug interactions."
The item set closes out with an overall rating items,
which asks respondents how satisfied or dissatisfied
are you with your hospital's EHR system?
You can see here only 6% are very satisfied
with the EHR system.
If you combine it to very satisfied and satisfied
we get 45% of respondents.
And then you can see the distribution where 33%
are neither satisfied or dissatisfied.
15% are dissatisfied, and 7% are very dissatisfied.
And the quotes speak to this.
"The EHR system at our hospital is the worst
EHR system I have ever used."
"EHR is not user friendly."
"There are too many issues, absolutely not user friendly
and potentially can cause serious issues."
I just briefly went over the results,
which are also available in the Pilot Study Results Report
on the AHRQ Web site.
Also on the Web site are the items available
both in English and Spanish.
In addition, there's a resource list,
which contains links to practical resources
to improve patient safety as it relates
to the use of Health IT in hospitals.
That resource list is organized by the measures
in the item set and it has things on how to improve alert
fatigue, or the safe use of copy and paste.
There is also a data entry and analysis tool.
That is an Excel-based tool.
Therefore, if you wanted to administer the item set
you could data enter it into this Excel tool
and it automatically calculates the scores for you
for each item and compares it to the pilot results.
The good news is that during the next
Hospital SOPS data submission in 2019,
AHRQ will be collecting the Health IT
Patient Safety item set data.
In order to get this data you would administer
the hospital SOPS data with the Health IT
patient safety supplemental items at the end.
And we would ask that you include the filter questions
at the beginning so that those who might not use
the EHR or not review information in the EHR
they can go ahead and skip out of the supplemental items.
A benefit of submitting to the database
is that you would receive a customized feedback report
that displays your results in addition to that
of the database, and also your results would
be included in aggregate into a database report
that would go onto the AHRQ Web site.
To stay up to date and informed about when
that data submission will occur or any news
about the Surveys on Patient Safety Culture in general
you can go to the AHRQ Web site.
In the top banner you'll see email updates,
and if you scroll down there's a lot
that you can stay updated on.
If you scroll down the Surveys on Patient Safety Culture
you'll be able to sign up for updates
by the various survey settings.
For example, hospital or medical office,
nursing homes, pharmacies.
And with that I think I'll send it back to you Joann,
and thank you.
- [Joann] Thanks, Naomi.
We're gonna now switch to the Q&A portion of the Webcast.
As a reminder you can type a question in the Q&A box,
which is shown on the slide.
To access the Q&A box you may need to select
the button with the three dots at the bottom
of your screen and select the question mark Q&A
for it to appear on the right panel of your screen.
Be sure to send your question to all panelists,
and feel free to share your name and/or organization or role
when you type your question.
Depending on the browser you're using,
your WebEx screen may look slightly different
from the slide.
So at this time please submit your questions
through the Q&A box.
I see during the webcast we did have a few questions
submitted and for our speakers, I'll let you know
if any of these questions are targeted for you.
But those that I can answer I will answer.
The first question we received was: "For the
composite measures are the questions equally weighted?"
And yes, the answer is yes.
For those composites where they consisted of three items,
the scores for those items would then be
the percent positive scores would be calculated
and then averaged across to come up with
the composite score.
The next question was: "Can we administer
the Health IT item set as a standalone survey?"
I just want to say the supplemental items
were designed for use with the core Hospital Survey
on Patient Safety Culture.
So they should be added at the end
of the Hospital SOPS survey.
More specifically you would add these Health IT items
between section G, which is number of events reported,
section H background information,
which is at the very end of the survey.
You'll also be sure to include the initial
filter question and any subheadings.
Another question we received was: "Is it possible
to include select items from the Health IT
Supplemental Item Set and not the whole item set?"
Our answer to that is that the supplemental item set
is intended for those who enter or review
patient information in your hospital's EHR.
And it was not designed to be completed by staff
in your hospital's IT or clinical informatics departments.
So what we recommend is that you use the questions
that are associated with the composites
and that you administer all of those questions
because that way you'll be able to compare
your results to the composite level results.
Another question: "What other supplemental item sets
are there for SOPS surveys?"
In addition to the Health IT Supplemental Item Set
for the Hospital Survey there's also
a supplemental item set on value and efficiency
for hospitals and medical offices.
And the value and efficiency item set
assesses the extent to which organizations
place a priority on and adopts practices
to promote efficiency, waste reduction,
patient-centeredness and high quality care
at a reasonable cost.
As a reminder, again, you can submit your questions
through the Q&A in the browser.
And again, your free to submit your questions at any time.
Another question that we're receiving
is: "When will the Hospital Survey of Patient Safety Culture
Version 2.0 be released?"
AHRQ and Westat are currently doing more cognitive
testing of the survey items
and will be conducting a pilot test.
We're expecting to release the updated version in 2019,
most likely in the Summer of 2019.
AHRQ will keep everyone posted on data submission dates
for the hospital database as we get closer
to those dates and at that time the Health IT items
can be submitted along with the hospital survey data
in the hospital database.
Let's see, the next question I'm seeing here,
will these supplemental items be revised
or are they compatible when the new
hospital Version 2.0 survey is available?
At this time, there's no plan to revise
these Health IT items.
These will be able to be added to the end
of either the current Hospital Survey on Patient Safety
Culture or the Version 2.0 when it is made available.
Next question is: "We are surveying this Fall,
and then adopting a new EHR before the next survey cycle.
Do you think it would beneficial to add
the Health IT supplement this Fall,
and then to survey after implementation
to measure for improvement?"
Naomi Yount, would you like to answer that question?
So again, there's a user who's surveying this Fall,
then adopting a new EHR
and could potentially survey again.
So would you recommend that they administer the survey,
the Health IT items, this Fall
and then again after implementation?
- [Naomi] Hi, thank you.
Yeah, I think you could do that.
In general, when we did the pilot,
when we were in the middle of doing it,
we would recommend not administering the survey
as people are learning the new or transitioning over.
But if you're going to do it in the Fall,
and you want to administer it now
before you've started that process
and then again after, maybe six months after,
I think that would be fine.
Joann, did you want to add to that?
- [Joann] No, I don't think so.
Okay, another question, this is for Dr. Brady.
"What do you find most interesting or exciting
about the Health IT items set
from a patient safety perspective?"
- [Jeff] Yeah, thank you, Joann.
I think my answer on this is not much different
than the full set of surveys.
It's just more directly applicable
to health information technology.
I think Tejal and Naomi did a great job
of describing all the different facets of this issue.
In general, I think most hear about these
with respect to either provider burnout
or just the technical challenges of implementing
health information technology and managing
this information rich process that we have in health care.
I think what's most exciting to me about the surveys
is they really help translate that awareness
of the fact that there are some challenges
and even big problems here,
some of which have a direct impact on safety.
To translate that awareness and move from anecdote
to action at the organizational level.
It's really important because every organization
is not necessarily the same.
The issues may be different.
One may be having more issues with duplicate entry.
That's one of the items on the survey.
We have to enter information in too many places.
Another may have more of a challenge with
excessive alerts or flags.
I think to really manage two of the current problems
and appropriately prioritize limited resources,
it's important for each organization to know that
that kind of information from their staff's perspective.
So again, just the ability to translate
that general awareness into more specific action
is what really impresses me the most.
- [Joann] Great, thank you for offering that perspective.
Next question I'm gonna send to you, Tejal,
and it's about the fact that the Health IT
supplemental item set doesn't specifically address
this issue of Just Culture or punishment and blame.
Does punishment and blame have a role
as it relates to Health IT culture?
And how do you think about Just Culture
as it relates to Health IT use and Health IT culture?
- [Tejal] Sure.
I think Just Culture does have relevance,
and I know there's components of that
that are present on the main SOPS survey.
But certainly when you're thinking about HIT,
particularly if an error occurs,
I think it's really important when doing
the deep dive into why those errors occur
to really go, again, like we do with any safety event,
beyond blame and punishment in terms of
the clinician didn't do XYZ with the technology correctly,
so let's blame the clinician.
We don't want to stop there.
We want to actually say why didn't they use
the technology as it was intended,
and are there usability issues
or training issues or other things.
So I think we still are seeing that organizations
essentially are blaming the user as opposed
to really digging deeper into what were
the contributing factors that led to the potential
misuse or erroneous use of that technology.
- [Joann] Yeah, those are great points,
and I don't know if, Jeff or Naomi,
you have anything you want to add to Tejal's comments
on Just Culture as it relates to Health IT.
- [Jeff] Naomi, anything you'd want to add first?
- [Naomi] No, go right ahead.
- [Jeff] Sure, yeah.
I think just focusing on maybe one section
to add some detail to Tejal's answer,
which I completely agree with,
I think a big part of culture that we know
that's important for patient safety is respect
and responsiveness and while those words aren't used
explicitly in the survey, I definitely can see
those concepts represented in items like
problems with our EHR system
are resolved in a timely manner,
or we're made aware of issues with our EHR system,
again thinking about these kinds of responses
from a staff perspective.
A lot of what's embedded in the way that they
answer those questions has to do with respect
and responsiveness and just recognition that
what frontline clinicians see
is critically important to patient safety.
I mean, this is a high reliability concept
that is fundamental to that conceptual frame.
So again, I think I could see how it's a bit harder
to trace the connections of blame and punishment
in comparison to the other sets of tools
in the patient safety culture survey.
But I think they are definitely here in
health information technology as well.
- [Joann] Great, that's actually, that's quite helpful.
Thank you for offering that perspective.
Two other questions here more around use of the survey.
"Can these Health IT questions be used
in a medical office population that has an EMR?"
Naomi, would you like to answer that question?
- [Naomi] Sure.
What we can say is that it has not been tested
in the medical office setting,
and not all the items may be relevant.
So I think we can't say no, don't use them there,
because there are probably many items that are relevant.
But they have not been tested in that setting.
- [Joann] Okay, great.
And then I think we have one final question.
"Will AHRQ also be accepting submissions
for the value and efficiency supplemental items?"
And what we can say is that yes,
we're working on that and so the expectation
is that when the hospital database is open
for submission that both the Health IT item set
and the Value and Efficiency item sets will be
able to be submitted at that time.
And it looks like we're able
to get through all the questions.
So we are basically at the end of our time.
So, great.
And I just want to say that thank you
to everyone for attending.
Thanks to our speakers.
A brief Webcast evaluation will be pop up
when you close out from today's Webcast.
So we encourage you to please take a moment
to provide us your feedback as it helps us
improve our offerings and plan future events
that meet your needs.
We also invite you to visit the AHRQ Web site
and contact us at any time by email or phone
if you have additional questions
or need technical assistance.
So thanks again so much to our speakers today
for this Webcast and thanks for joining us.
This concludes today's presentation.




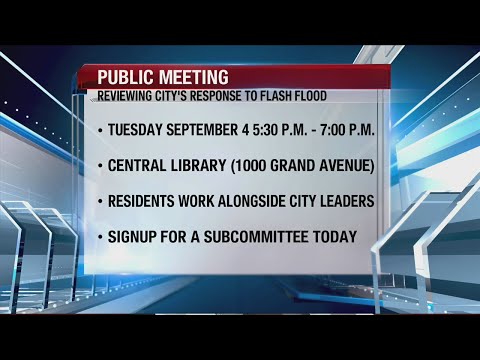 For more infomation >> The city of Des Moines is looking for your input on their performance - Duration: 2:29.
For more infomation >> The city of Des Moines is looking for your input on their performance - Duration: 2:29. 


 For more infomation >> Plans for new childcare option that would focus on working women in tech in the works - Duration: 1:45.
For more infomation >> Plans for new childcare option that would focus on working women in tech in the works - Duration: 1:45. 

 For more infomation >> Congratulations to Nalarence Davis for being the 18th caller and winning a Michael Kors purse - Duration: 0:43.
For more infomation >> Congratulations to Nalarence Davis for being the 18th caller and winning a Michael Kors purse - Duration: 0:43.  For more infomation >> Philippine President Rodrigo Duterte defends choice for new chief justice - Duration: 0:59.
For more infomation >> Philippine President Rodrigo Duterte defends choice for new chief justice - Duration: 0:59.  For more infomation >> Health Headlines for Aug. 28, 2018 - Duration: 2:31.
For more infomation >> Health Headlines for Aug. 28, 2018 - Duration: 2:31. 


Không có nhận xét nào:
Đăng nhận xét